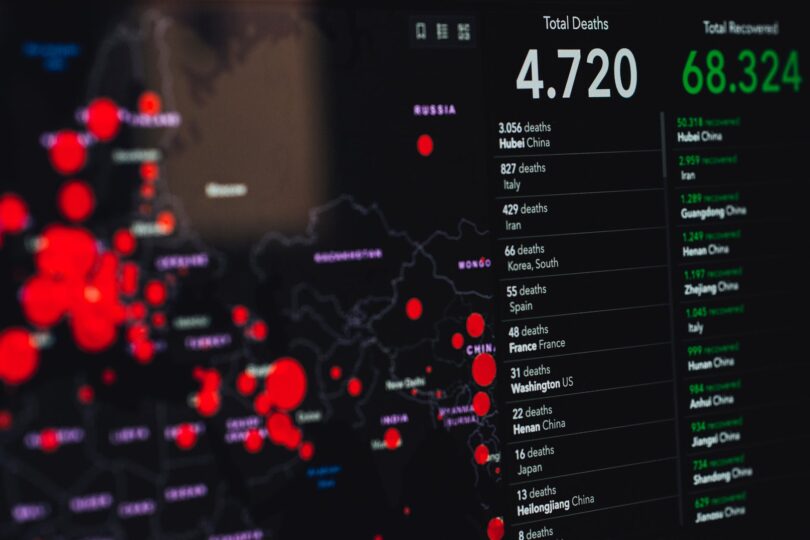
As CNBC reported, the first Chief Medical Officer of the US Government, a former executive of IBM Watson Health, wants his new role to help place software companies like Palantir Technologies in the hands of researchers that can use the company’s technology to make smart decisions for the next pandemic. In this issue we focus on understanding the long-term impact of the COVID 19 pandemic and begin to learn lessons from the mistakes made in addressing the current health crisis to prepare for future crises. By providing policy, practice and learning recommendations from the perspective of health systems, this article provides the basis for the necessary interdisciplinary research and real policy discussions to prepare health systems for future pandemics.
A comprehensive review of the response to the current COVID 19 pandemic on all levels has identified gaps, challenges and successes. These results need to be incorporated into future planning to improve preparedness and response to the next pandemic. Here are seven areas where we can learn from our COVID / 19 response to improve preparedness for future pandemic shocks.
As COVID 19 rages round the world, it is not too early for companies and countries to apply the lessons of the pandemic to prepare for the next one. To prepare for this or the next viral pandemic, governments and NGOs must focus on preparing health infrastructure, monitoring viruses, and predicting the next outbreak. The coronavirus pandemic has opened a window of opportunity to rethink how countries prepare for health crises.
During the time that the world recovers from the COVID-19 pandemic, experts in public health and emergency management are preparing for the next one. One year has passed since the World Health Organization declared the Coronavirus pandemic a global pandemic on 11 March 2020. But while people are still frightened of Covid-19 and thinking about how to wash their hands, the next public health emergency management expert is preparing for it.
The pandemic of coronavirus has exposed the mutual vulnerability and lack of preparation for the spread of catastrophic infectious diseases in Europe and the United States. In response, many governments have shown a lack of preparedness in the face of a systemic global health crisis. The World Health Organization ranks the flu pandemic and other highly dangerous viral diseases such as Ebola and Dengue among the top ten threats to public health.
The COVID 19 pandemic has highlighted the extreme complexity of managing a systemic and global health crisis. The vulnerability of an uncompetitive and ill-prepared US health care system, with over 26 million people in the system as well as the uninsured and underinsured, became apparent during the pandemic. The pandemic highlighted and exacerbated a number of challenges that relate to health workers’ availability, distribution, training, safety and protection.
Government failure manifested itself in the spread of misinformation and mistrust of science and health workers, and the subsequent failure to take public-health measures that could have saved lives and contained the pandemic. Building resilience to pandemics is not only a matter of strengthening global disease surveillance systems and improving government responses or of building hospitals and infrastructure, it is also a matter of ensuring that individuals and households have what they need. A clear sense of how to prepare for the next pandemic requires a deep dive into these failures, understanding of what went wrong, and work to improve the architecture of health security and governance – a point raised by John Nkengasong.
The need to plan and prepare for an overwhelming outbreak of infections, such as the next flu pandemic or Ebola epidemic, poses new challenges to the practice of pediatric intensive care. Planning pediatric care during a pandemic is imperfect, and offers no relationship between flexibility and knowledge of how to adapt to changing threats. This means that governments must launch a campaign to help households by providing them with the information and resources they need to prepare for the next pandemic before it occurs.
The onset of the next major pandemic will affect our ability to deliver the traditional approaches to a large number of patients. As we prepare for the next pandemic we will be forced to change our medical decision making system with limited resources that are not what we are used to, especially in developing countries.
Medicare will allow us to address the social determinants of health by focusing on prevention, primary care, chronic disease management and special care. It also needs to protect victims of the next pandemic from the devastating financial consequences of disease through affordable, high-quality health insurance.
One practical way to prepare for a future pandemic is to ensure that the system structure remains stable. A robust public health system enables us to implement the types of surveillance, tracking, tracking, and data collection that are critical to responding to a pandemic or other emerging public health crisis.
A public-private approach can catalyze national and global resilience to emerging threats such as climate change, pandemic preparedness, bio-defense and other effective resource use to manage catastrophic events and plans. Public and private funding for these efforts will demonstrate commitment to global health care and provide a defense against future pandemics that is science-based and independent of political rhetoric.
Even at a tiny fraction of the cost of our $1.9 trillion COVID-19 stimulus package, we can strengthen our collective vulnerability by investing in systems that help households cope with the ongoing uncertainty of the current pandemic and be more resilient to future pandemics. One way to do this would be to increase the supply of products to health systems that struggled to find their source during the current Covid 19 pandemic.